Is COVID More Dangerous Than the Flu?
Unpacking The "Science" Behind the Annual Vaccination Scam
Story at a Glance:
•A huge business exists that revolves around making people afraid of the seasonal flu so vaccines can be sold each year.
•Many of the fundamental ideas supporting this practice are erroneous or rest on a very shaky foundation—for example, no one actually knows how dangerous the flu is and flu shots have been shown to make you more likely to become ill from the flu.
•Much of the COVID-19 playbook was copied from the one developed to sell flu shots. For this reason, understanding the malfeasance with the influenza vaccination program provides a valuable context for understanding what is happening right now and why treatments for these conditions are never allowed to see the light of day.
Recently, I was consulted by a public figure to answer a seemingly simple question—is COVID-19 less deadly than the flu now?
Unfortunately, this is actually a very difficult question to answer, to the point I would have never imagined how difficult it was had I not looked into it myself. After I reviewed the data with the public figure, I realized that there is a lot of value in exploring that answer with each of you as it cuts to the heart of the pandemic industrial complex.
Note: this article was recently published on Mercola.com—a website I have read for decades. It has been slightly revised since the initial publication.
The Influenza Industry
For more years than I can count, I’ve watched the same script be re-enacted:
1. We are warned it’s going to be a bad flu season.
2. We are told it is thus essential to get our flu shots by every media network and health authority we encounter (along with the majority of healthcare workers we see).
3. The flu shot to varying degrees “fails” because it doesn’t quite match the circulating strain of influenza.
4. We are told the flu season will be extra bad because the flu-shot isn’t for the correct strain, but it is nonetheless essential to get your flu shot because the partial protection it provides is still lifesaving.
5. In bad years (which is many of them), understaffed hospitals get over crowded, which in turn is used to whip up a hysteria to justify doing even more to push that year’s vaccines.
6. The flu season ends and we are told it killed a lot of people and that we must work harder to vaccinate next year so this does not happen again.
Note: points 4 and 5 are frequent but do not happen every year.
The most recent example of this occurred right before COVID-19:
Note: as the above article shows, hospitals running out of beds like we saw throughout COVID-19 (which was the initial justification for the disastrous lockdowns) is a longstanding issue resulting from chronic understaffing issues.
In accordance with the sales script, during the 2017-2018 flu season every health authority promoted the vaccine—despite noting it had once again not correctly predicted that year’s strain. Yet, was this actually a good idea?
Between September 2017 and February 2018, influenza A(H1N1)pdm09, A(H3N2) and B viruses (mainly B/Yamagata, not included in 2017/18 trivalent vaccines) co-circulated in Europe. Interim results from five European studies indicate that, in all age groups, 2017/18 influenza vaccine effectiveness was 25 to 52% against any influenza, 55 to 68% against influenza A(H1N1)pdm09, -42 to 7% against influenza A(H3N2) and 36 to 54% against influenza B. 2017/18 influenza vaccine should be promoted where influenza still circulates.
During that flu season, I clearly recalled that each patient I saw who had been hospitalized or put onto a ventilator had received that year’s flu shot, whereas no one I knew who had not vaccinated had any issues with that year’s flu. While my observations may have been anecdotal, they are in fact supported by the previously cited study because:
The most identified strain of the virus is influenza A (H3N2). According to a CDC emergency health advisory released Dec. 27, 83 percent of reported cases were H3N2, a strain associated with more hospitalizations and deaths in those over 65 years of age and in young children compared to other age groups.
Or put differently, the vaccine made you roughly 17.5% more likely to catch the dangerous strain that characterized most of the flu season. However, this did not in any way stop anyone from pushing that vaccine—and I still remember the numerous mind-boggling debates I had with pulmonologists about it, something I believe illustrates how invested their profession is in this approach.
Likewise, it seems no degree of data can change their minds. For example, a 2013 Cochrane Review (which was the most definitive way to assess the existing medical evidence—at least until the group got bought out by the Gates Foundation) found:
We could find no convincing evidence that [giving children] vaccines [for influenza] can reduce mortality, hospital admissions, serious complications or community transmission of influenza…Despite the great variety of method variations, the reviews all have similar conclusions to those of our 2005 Cochrane Review: trivalent inactivated vaccination has few effects and there is no evidence that it affects deaths, complications or transmission of influenza. Live attenuated vaccination performed a little better at the expense of safety.
Likewise, numerous studies (some of which were compiled in this article illustrating how vaccines frequently increase rather than decrease infectious diseases) have shown that influenza vaccines increase your risk of catching influenza, catching other respiratory viral infections, and developing a severe influenza infection. Worse still, that elevated risk of illness persists in the years that follow receiving an influenza vaccine.
“Treating” Influenza
Given the total inefficacy of the vaccine, this suggests that a better approach might be to:
•Reduce individual susceptibility to the flu.
•Have home treatments (e.g., over the counter ones) for the flu available to the populace.
•Have effective treatments be available to healthcare providers to treat patients with the flu.
However while many such treatments exist, they are always marginalized and often attacked by the medical community.
For example, it has been repeatedly observed that influenza outbreaks tend to occur in tandem with low levels of sunlight, suggesting a vitamin D deficiency is a causative factor for influenza. In turn, a significant amount of research has been done between vitamin D levels and the flu. Consider the following:
A study measured the vitamin D concentrations in 198 healthy adults each month during the fall and winter of 2009-2010. It found the incidence of infection was 2.7 times lower and the percentage of days ill was 4.9 times lower in the group that maintained vitamin D levels of 38 ng/mL or higher during the entire study period as compared to the group with levels below 38 ng/mL
A meta-analysis of eleven placebo-controlled studies containing 5,660 participants (of 6 months to 75 years of age) found that oral vitamin D supplementation caused a 36% reduction in the risk of both upper and lower respiratory tract infections (e.g., influenza and Streptococcus pneumoniae).
A meta-analysis of five placebo trials found vitamin D supplementation reduced the number of respiratory tract infections in adults by 35% and in children by 42% when compared to groups that did not receive supplementation.
Yet, vitamin D is never suggested for the flu, and frequently the recommendation is attacked. A similar treatment is also extended by the medical profession to many other long used natural treatments for influenza (many of which I have found to be extremely useful—to the point I have never viewed the infection as being problematic).
Conversely, the conventional management of influenza typically consists of:
•Telling the patients to stay hydrated.
•Telling the patients to take the doctor’s preferred fever medicine (which is typically tylenol or ibuprofen).
•If the patient has had the flu for two days or less, prescribing tamiflu.
Unfortunately there are some issues with these approaches.
Suppressing Fevers
In the case of fevers, a long standing belief in the natural medicine community has been that suppressing fevers worsens your body’s immune response and its attempts to expel an infection, so the natural medicine field strongly advises against suppressing fevers. This for example was clearly demonstrated throughout the devastating 1918 influenza pandemic and many reports at the time showed it determined if a patient would live or die.
From reading all of these reports, (provided the fever is not too high) I’ve adopted the practice of instead often encouraging fevers during these types of infections and found it frequently significantly improves how quickly the patient recovers. Furthermore, I also found that for some patients, a significant amount of the discomfort they experience during an illness comes not from its fever, but rather the body struggling to heat itself up to the target temperature needed for the fever. For this reason, I often find (provided the patient is not on the frail end), that to reduce discomfort it is more effective to heat the body up (e.g., with an infrared mat) than it is to use a medicine which suppresses the fever by turning off the body’s signal to heat itself up.
However, since the response with a fever reducing medication is immediate and dramatic (thus being something simple to do which showcases the efficacy of pharmaceutical focused medicine), the medical profession has always been attached to treating fevers. In turn, a variety of conflicting data exists on if suppressing a fever worsens the course of an illness or makes it more likely to be transmitted, and as you might expect, whenever data emerges suggesting fever suppression is harmful, it’s repeatedly attacked. For example, this study, this study and this study support my position while this study (from a very orthodox journal) opposes it.
Since there is so much conflicting data, I’ve gone off my own personal experience where it’s often been quite clear that suppressing fevers worsens the course of these illnesses while doing things like going in a sauna greatly accelerates the speed with which you clear them.
Note: early in the pandemic, the French health ministry warned against using ibuprofen to treat COVID-19 after observing numerous cases where it worsened the course of a COVID-19 infection—a decision that was repeatedly criticized by the medical community. My own experience matches that of the ministry, as I’ve seen quite a few patients become much worse after they started a medication to suppress their fever and I’ve also seen others respond to their bodies being warmed up.
Tamiflu
The more I study medicine, the more I’ve come to believe that business rather than science dictates what governs how medicine is practiced. For instance, any illness that regularly affects a large number of people represents a huge potential market to sell medical products, and as a result, the industry has a vested interest in keeping anything which actually solves a health issue (and thereby destroys that market) from becoming available to the public.
In the case of the flu (and related viral illnesses) since people get it every year and feel miserable (hence wanting something to be done for them), there has been a longstanding need to protect that market. As a result, each therapy that is sanctioned for “solving” it (e.g., the annual vaccines) at best does a small enough amount that the market is not threatened. Conversely, ways to treat the illness (many of which, like vitamin D, can be obtained for minimal cost) are continually suppressed. Because of this, I live in a bit of a surreal reality—I do not feel the flu is a big deal and am never worried if I or my friends get it; but I simultaneously recognize many of my physician colleagues are terrified of it and that in a susceptible person, if it is not handled correctly, it can become a huge problem.
In 1999, Roche’s Oseltamivir (Tamiflu), an influenza treatment was approved by the FDA and in 2002, by the EMA. When Tamiflu first hit the market, it was enthusiastically endorsed by the medical profession, while its significant rate of side effects was glossed over—1 in every 19 to 22 people (depending on age) treated experienced vomiting, 1 in 28 experienced nausea, 1 in 94 experienced a significant psychiatric event, and a variety of rarer but more severe side effects like kidney or liver damage were also observed with the drug.
Because of the fanfare surrounding Tamiflu, by 2009, Roche had been able to convince the European and American governments to spend billions stockpiling it. However, most of that fanfare was based upon studies Roche had conducted that they refused to reveal to the public or independent researchers. When the Cochrane Collaboration eventually obtained access to that data (e.g., through FOIA requests) they discovered that Roche’s data showed Tamiflu offered almost no benefit to patients while simultaneously presented a moderate risk to them.
One of my longterm observations has been that once the government invests a lot of money in something (e.g., more than a billion dollars to buy the entire supply of remdesivir and over 30 billion on the COVID vaccines), it becomes extremely committed to the investment. This means that it will do everything it can to utilize that investment (e.g., by administering the purchased pharmaceuticals to the population) and if evidence comes up suggesting the investment was a bad idea, the government will willfully disregard it.
In the case of Tamiflu, once evidence started emerging it was a scam, rather than acknowledge it, the healthcare authorities like the CDC chose to ignore it. This has created the curious situation where Tamiflu (and related medications) are the standard of care for treating influenza, but, there is no evidence to justify that position. As a result, when you read the CDC’s most current guidelines, you will notice a curious contradiction. They advocate for the medication, but simultaneously use speculative language to avoid being caught in a lie:
If you get sick with flu, influenza antiviral drugs may be a treatment option….Check with your doctor promptly if you are at higher risk of serious flu complications and you get flu symptoms….When treatment is started within 1-2 days after flu symptoms begin, influenza antiviral drugs can lessen symptoms and shorten the time you are sick by 1 or 2 days. They might also prevent some flu complications, like pneumonia. For people at higher risk of serious flu complications, treatment with influenza antiviral drugs can mean the difference between milder or more serious illness possibly resulting in a hospital stay.
Note: the above language is potentially appropriate for a brand new drug approved under emergency situations—Tamiflu however has been on the market for 24 years.
When COVID started in December 2019, I correctly predicted give or take everything that would happen in the years to come. At the time my colleagues didn’t believe me (and often attacked me for my position), but have since come around and apologized since the predicted events did come to pass.
On the surface, it seems nearly impossible I actually could have made the predictions I just claimed to have made. However, if you consider the medical community’s insistence on making the flu out to be an existential threat and its steadfast refusal to turn influenza into an easily manageable condition, it’s not much of a stretch to assume the exact same thing would happen with COVID. For instance, this was why I strongly suspected adequate vitamin D would be critical for COVID but nonetheless be ridiculed and attacked regardless of how much evidence was put forward supporting its use. Likewise, I thought the Tamiflu saga would essential repeat with the new antiviral drugs they made for COVID (which is what then happened with remdesivir, paxlovid and molnupiravir), especially given that Fauci, who was in charge of the COVID-19 response had used a similar playbook during the early days of HIV to push through the toxic and ineffective drug AZT.
Overall, the strongest case for this argument can be found from Vaccine Zombie, a 2010 music video poking fun at the 2009 swine flu vaccination campaign. At the time it was made, it was meant to be an over-the-top caricature that highlighted the absurdity of the previous year. However, because the relentless greed of the industry was allowed to run unchecked, what had been unthinkable then became the new normal a mere decade later, and as a result, to a very eerie degree, Vaccine Zombie perfectly predicted what happened throughout the COVID-19 vaccination campaign.
What Drives the Vaccine Industry?
If we take a step back, it’s worth considering how effective the vaccine approach is. For example, in 1980, we gave 12 million flu shots each year in the United States, while in 2020, we gave nearly 200 million. Given this huge investment, you would expect to see a pretty large public benefit from it:
At this point, over half of the American population receives an annual flu shot, yet despite its clear failure to do anything (as the above graph shows—at best mass influenza vaccination has mitigated the effect of an aging population), the mantra is always the same. Not enough people are vaccinating and the most important thing you can do each year is to get vaccinated.
Given the abysmal failure of this program, I’ve always wondered why those vaccines are pushed so aggressively. At this point, I’ve identified the following possible explanations:
•It serves as an annual ritual to make the population (and healthcare workers who are often forced to vaccinate) be compliant with the medical system. This approach is a well-known psychological tactic and other versions of it have been used by numerous nefarious groups throughout history seeking to entrap others within their ideology.
•It serves as an ideal market for the industry since it guarantees a large volume of recurring revenue. Furthermore, as I was informed by a pharmaceutical executive I’ve corresponded with, the price adult vaccines are priced at makes their profit margins be irresistible to the industry.
Note: one reference I found estimated the cheapest influenza vaccines cost 0.20 per dose to produce and when averaged with the rest (which includes many experimental and thus more expensive vaccines), cost 3.30 to produce. Conversely, the CDC currently pays between $13.92 to $19.03 per dose of an influenza vaccine, while the private sector pays between $18.43 to $30.10 for each dose. This adds up to a lot given that half the population receives one or more of these products each year.
•Each branch of the federal government has to continually fight for its funding. One of the classic approaches the CDC (and related agencies) use to justify their budget is hyping up the hysteria about infectious disease outbreaks and the need for those agencies to protect us. Because this script works (as most congressmen have minimal knowledge of vaccination or epidemiology), each year we see a similar one be deployed throughout the media by experts from each of those branches who promotes the need for everyone to vaccinate.
Note: in addition to fighting for a piece of the federal budget, many of the agencies also depend upon their relevant industry to fund them (e.g., the pharmaceutical industry pays 45% of the FDA’s budget). In the case of the CDC, after Congress in 1983 authorized the agency to take money from the private sector, there have been numerous complaints from CDC employees, outside watchdogs and congressmen over the resulting corruption (summarized here). As the CDC is the most dependable promoters of vaccinations, it should come as no surprise some of its largest donors have been the COVID-19 vaccine manufacturers.
•The nation’s vaccine production cannot be paused and then restarted. For this reason, the Department of Defense has made the decision annual vaccinations need to be produced for America so that those production facilities can be available to produce emergency vaccines if a bioterrorism event occurs that gravely threatens national security. While I understand why many in the political leadership seriously believe this, I believe they are extremely misguided as it is simply not possible to reliably address a dangerous novel pathogen with a vaccination (most recently demonstrated with COVID-19), whereas it is very feasible to do so with repurposing existing medical treatments (again also demonstrated throughout COVID-19).
•Over the years I’ve seen numerous cases be presented that argue the goal of an annual vaccination program is to harm the recipients and create illness in society (e.g., because a lot of money is made from treating the autoimmune disorders vaccinations create). This is one possible explanation for why our authorities continually ignore the evidence showing vaccines do more harm than good—but at the same time, it’s quite speculative and the previous explanations also suffice to explain the rigid adherence to the current paradigm.
How Dangerous Is The Flu?
As the previous sections illustrate, given how deeply many parties are invested in the influenza industry, it’s within the realm of possibility those same parties (e.g., the CDC) might exaggerate the severity of the flu season. Some of the ways they are commonly alleged to do it include:
•Labeling respiratory diseases as influenza when they are actually due to another virus which creates similar symptoms.
•Categorizing deaths as being from influenza that were most likely completely unrelated to the infection (e.g., a heart attack).
•Categorizing frail people (e.g., those who were expected to die soon) who died as the result of an influenza tipping them over the edge as an influenza death.
•Not counting the vast number of people who catch the virus and develop a minor or non-existent case of it (thereby making the dangerous outcomes appear to be much more frequent than they actually are).
You might recognize some of these since, once again, the same tactics were also used throughout COVID-19.
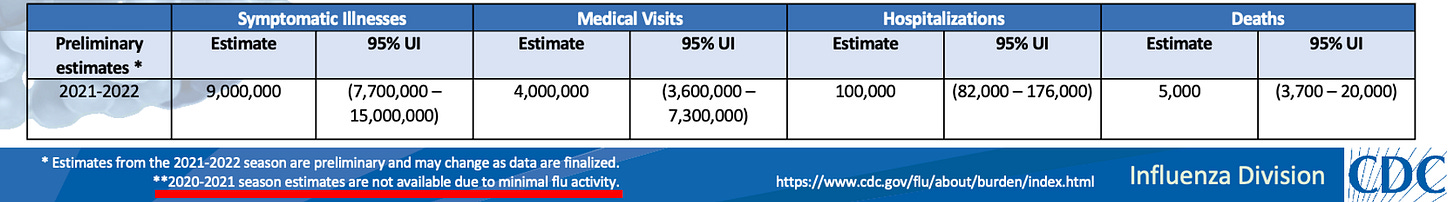
This in turn has led to a long standing question; how many people actually die each year from the flu, and how many deaths are simply deaths that would have occurred anyways being relabeled as influenza deaths. Let’s for a moment consider, the CDC’s influnenza estimates:
Yet during COVID, most of these suddenly disappeared:
Let’s also quickly compare the influenza numbers to what was observed during COVID:
Note: I created the above table from this, this, and this CDC dataset.
Given that, per the CDC, influenza virtually disappeared during COVID-19, this almost certainly means the CDC has done one or more of the following:
•Erroneously attributed hospitalizations and deaths to influenza and COVID-19 which were in fact due to something else. Since those deaths were independent of an influenza infection, this explains why they could be shuttled over to the COVID-19 category.
•Erroneously classified hospitalizations and deaths from influenza as being from COVID-19 (thereby inflating the COVID numbers). This was most likely due to the fact a bias existed with medical providers to only test for or diagnose COVID-19 during the pandemic (partly due to the existing financial incentives to diagnose things as COVID-19), so influenza was never tested for and labeled as a cause of death.
Before I go further, I want to note that these numbers are estimates, and that the CDC admits when they calculate the annual impact of the flu, many of the deaths never had a positive influenza test before they died nor was influenza listed on the death certificate. Instead, the CDC tries to account for the numerous flu cases they believe were there but no one recognized (e.g., you got the flu and then had a heart attack a month later). A short explanation of their methodology can be found here, and a longer one here.
From reviewing that methodology, my own opinion is this approach likely inflates the number of deaths from the influenza. Furthermore, from looking at the CDC’s data, I’ve seen numerous cases where very different death rates are provided (e.g., over 80,000 deaths claimed here for 2017-2018 flu season verses the 52,000 that were claimed here).
All of this in turn circles back to a central question—how dangerous is the flu?
My own experience and that of many of my colleagues has been that in many parts of the country, you will only occasionally see patients who were hospitalized for the flu and in most cases, those hospitalizations are for a bacterial pneumonia which followed the original infection. Conversely, in certain places (particularly New York), each winter, large waves of older adults are hospitalized for the flu and frequently die.
Note: there was a moderate overlap between the map of the COVID-19 death rates and influenza death rates by state. Likewise, the state most severely affected by COVID (New York) also was always one of the worst hit states for influenza and pneumonia.
In short, although we push the same approach for mitigating influenza on everyone (along with the related conditions we misdiagnose as influenza), the reality is the disease can’t be viewed as a single condition. For example, in areas like New York City which are known to have a large number of elderly residents who are killed by the flu each year, some of the hysteria around influenza is in fact justified, while in other locations it’s simply not. Likewise, sunlight exposure and vitamin D levels should always be evaluated when determining how aggressive the measures to mitigate the flu should be for an area—however since something as simple as supplementing vitamin D to those at risk is never on the table, an idea like the one I just proposed would never been up for consideration either.
There are also a variety of medical conditions that are associated with an increased risk for a fatal influenza infection (and more importantly, the pneumonia which follows and is much more likely to be the cause of death). Chronic obstructive pulmonary disease (COPD) is one of the most well known examples, and in turn, doctors usually identify those patients and encourage them to do extra measures like taking the pneumococcal vaccine.
To elaborate, COPD is one of the top causes of death in the United States (causing over 150,000 deaths annually) and viewed as a gradual but inevitable progression to death for those who have it. One of the many things which causes COPD patients to die is pneumonia (partly because they have to take inhaled steroids which suppress the lung’s ability to defend itself from invaders), which often raises the question of “Did a prior influenza infection kill this patient?” since fatal pneumonias (along with a variety of other fatal events) still occurs in the absence of influenza.
Note: the COPD situation is quite tragic (except for the drug companies) because the existing pharmaceuticals for it can slow the progression of the disease, but cannot stop it, leading to it eventually being fatal (and often quite miserable at the end). However, nebulized glutathione can halt the progression of COPD (discussed further here), and this has been known for decades, but since so much money is made from selling COPD meds for the rest of a patient’s life, almost no one knows about this un-patentable approach.
Although many risk factors have been identified for a bad outcome from the flu, presently, I believe one of the most important ones is a diminished physiologic zeta potential—the electrical property of the body which prevents things inside fluids (e.g. blood) from clumping together (which amongst other things can cause microstrokes).
The human body evolved to have a zeta potential which is a bit above what causes blood to begin clumping together, an adaptation that allows blood to clot soon after a vessel is punctured (thereby preventing fatal bleeding) while simultaneously not clotting within the vessels under normal conditions (which is essential for life). However, many thing that have been introduced to our environment push us towards that clumping state, and both I and many of my colleagues believe this loss of zeta potential is the root cause of many modern diseases.
Two of the most effective agents for creating that clumping effect are aluminum and the SARS-CoV-2 spike protein. In the case of aluminum, this property is widely utilized (e.g., to separate fecal matter from sewage in water), and a strong case can be made that childhood vaccines injuries (e.g., sudden infant deaths) are due to microstrokes created from aluminum in the vaccines. Likewise, many of the unusual side effects from spike protein illnesses can be directly traced to a disruption of the physiologic zeta potential (which is often what needs to be treated to address those injuries).
Two other factors that also affect zeta potential are aging (it worsens as we age and I believe this is one of the underlying causes of the degeneration seen with aging) and acute infections like influenza. One individual who studied this extensively was able to observe a consistent drop in zeta potential when individuals got the flu, and could correlate the severity of their illness (e.g., feeling awful versus dying in the near future) to their pre-existing zeta potential, as when it was high, a drop could be tolerated, but when it was low, a further drop (induced by an infection) would create disastrous consequences for them.
I mention all of this because many of the annual vaccinations patients receive for influenza and pneumonia contain aluminum, I have admitted patients to the hospital who suffered a textbook zeta potential collapse after one of these vaccines, and many of my colleagues believe the repeated administrations of these vaccines plays a role in creating a weakened zeta potential that cannot tolerate the additional impact of an infection.
The Infection Fatality Rate
In order to assess if COVID-19 is more or less dangerous than influenza, we would want to know how likely an infection with each was to kill you (the infection fatality rate or IFR).
Note: Typically, the IFR is distinguished from the case fatality rate (IFR applies to everyone who had the disease, CFR only applies to those who had enough going on to be diagnosed). Typically the CFR is much higher than the IFR (e.g., those diagnosed with COVID at the hospital are understandably much more likely to die than someone who gets COVID and never notices it). However, since we diagnosed so many people with COVID on the basis of them having a positive test in the absence of symptoms (since we tested everyone), infections were classified as “cases.”
In the case of influenza, this is a surprisingly hard question to answer since as best as I can tell, no official estimate IFR has been ever produced (although the severe strains are commonly believed to have an IFR of around 0.1%).
Instead the CDC estimates how many people in total will die each year from it, calculating that 1.8 per 100,000 people will die from influenza while 16.3 per 100,000 will die from influenza and pneumonia. In order to have a death rate approximating the CDC’s number of annual influenza deaths, you would need to have a death rate of approximately 12.1 per 100,000 people, which again suggests the CDC’s figure at the start of the article is overestimating deaths from influenza by counting unrelated pneumonia ones within it.
If we use the CDC’s own figures of estimated number of influenza cases and total influenza deaths, we arrive at a CFR between 0.09% to 0.17% of symptomatic infections being fatal (so roughly 1 in 1000 people who gets the flu will die from it). The only formal estimates I’ve seen of the influenza IFR came from the 2009 Swine Flu epidemic—which I believe was made possible because of the intense media focus on it.
Note: the CDC’s eventual estimate for 2009 was that there were 60.8 million cases, 274,304 hospitalizations and 12,469 deaths. Assuming the same criteria was used to estimate this year (which it may not have been as most of the CDC’s published estimates only go back to the 2010-2011 flu season), this would have put it within range of the other influenza/pneumonia and given it a CFR of 0.2%.
Unfortunately, as the authors of a meta-analysis seeking to answer this question found, across 50 published studies assessing the CFR for the 2009 influenza, there were massive variations in the ultimate answer, ranging from CFRs of less than .001% to CFRs over 10%. Specifically, for laboratory confirmed cases, estimates ranged from 0–13,500 deaths per 100,000 infected (with 25 of the 29 estimates having a CFR between 0.1%-5%), and for symptomatic but not laboratory confirmed cases, estimates ranged from 0–1,200 deaths per 100,000 cases (with most of the estimates ranging from 0.005%-0.5%). For instance, there was a case in a New York school where 800 staff and students had an influenza like illness, but no one developed a severe illness, let alone died. The authors in turn concluded their paper by acknowledging we are not presently equipped to determine the CFR of an infectious virus:
A consensus is needed on how to define and measure the seriousness of infection before the next pandemic.
“It’s Just A Flu Bro”
Since so many people’s livelihoods depend on stoking the fears about infectious diseases, as I watched COVID-19 unfold in China at the end of 2019, my first thought was “it looks like the pandemic they’ve spend decades clamoring for has finally arrived.” I thus was taken aback when almost every public figure instead did the opposite, insisting what was happening in China was not a big deal, and then later argued that concerns about it were primarily born out of xenophobia.
Watching that unfold was what made me become convinced COVID-19 was going to turn into a global debacle as the only explanation I could see for this behavior was that it was already known COVID-19 was a major issue and it was being downplayed to either:
•Give the virus sufficient time to spread around the world so any possible window to contain it would be lost.
•Have time to prepare a response for the pandemic before public panic settled in—for example stockpiling personal protective equipment for healthcare workers before all of it was bought by the public.
Note: The Event 201 exercise (which can be viewed here) took place on October, 19 2019, was hosted by the Gates Foundation and The World Economic Forum, and was attended by many of the key parties that would later direct the COVID-19 response. It simulated the possibility of a novel SARS like virus spreading across the world, killing millions, and crippling the economy. After I learned of this exercise at the end of December 2019, I was struck by how accurately it (and later WHO conferences) repeatedly predicted much of what I would soon watch unfold (e.g., the exercise repeatedly called for social media companies to stop taking a neutral position on “misinformation” and censor everything that threatened the narrative). Much later, as the pieces came together, I learned that it was most likely known by mid-October that the Wuhan lab leak occurred—and curiously throughout the exercise, they kept on posing the question of how to address the public suspecting the virus was released by the pharmaceutical industry in order to sell a cure for it.
As a result of this systematic downplaying, all attempts made to mitigate the pandemic were attacked, and in many cases the Democratic leadership (e.g., New York City’s leadership and Nancy Pelosi) as a “sign of solidarity” actively promoted large social gatherings with people who had recently traveled to the United States from China and even Wuhan. This was quite curious as the most ardent opponents of containing the pandemic when it first began to spread in the United States later became the most ardent proponents of locking the country down once it had become too late to stop its spread.
One of the scripts I saw repeatedly be used (it was quite fascinating to watch it first diffuse online and then into the general media) was that COVID-19 was no worse than the flu. So, if you were actually hysterical enough to be worried about COVID, the most important thing you could do would be to chill out and get your flu shot, as a flu infection was a far more pressing concern and catching the flu would also make it more likely you would have a bad outcome with COVID-19.
Note: COVID-19 was not officially named until February 11, 2020—so it was not actually called COVID at the time much of the above took place.
This was awful advice which made no sense (later I even came across numerous pieces of evidence suggesting the 2019 flu shot made individuals in certain areas much more susceptible to COVID-19). Nonetheless, by February 2020, whenever I brought up COVID-19 with colleagues, all but two of them essentially repeated the above script back to me when I brought this subject up with them.
Those of us who tried to bring attention to COVID at this time in turn remembered all of this as the “it’s just a flu bro” period since that was essentially the response we’d get whenever we brought it up. Oddly, references to it have almost entirely vanished off the internet, but this is one such example you can still find.
Because of all the back and forth on if COVID was or was not more dangerous than the flu, I believe it left people very disoriented on the subject and often primed to dig into whichever position they had eventually committed themselves to (e.g., believing COVID was in fact just a bad flu).
Note: I also saw something similar happen with masks. Shortly before COVID arrived in America, I watched a public WHO broadcast which said safeguarding the global PPE supply (e.g., N-95 masks) for healthcare workers would be a top priority, and almost immediately afterwards, I watched every public health official suddenly say masks were pointless and unneeded. I concluded they were most likely lying to support the WHO directive and I immediately bought out the local PPE supply in my area. About a month later, PPE ran out across America, and I then mailed everything I had collected to my colleagues around the country (who had all disregarded my earlier advice to stock up on PPE).
Is COVID-19 More Dangerous Than The Flu?
Note: Although I feel the severity of COVID was greatly exaggerated, I also believe the early COVID variants (up to Delta) were extremely dangerous in certain people. For example, numerous people I’d known for years who never had issues with the flu nearly died from COVID (and likely would have without an integrative treatment protocol), many in my circle felt the infection was completely different from any other illness they’d had and my close colleagues in areas like New York City experienced waves of COVID-19 which were just as bad as the media portrayed it to be. Simultaneously, in many other areas, and for many of the people I knew who got it, COVID was indistinguishable from a minor flu. To this day, despite a lot of investigating, I have still not been able to explain why such radically different courses happened with the illness.
One of the things I find immensely fortunate about COVID-19 is that the sheer egregiousness of it motivated many researchers and journalists to start critically reviewing all the available data and questioning the unchallenged beliefs of the pandemic industrial complex.
For example, a major challenge in determining the IFR of a respiratory virus is that the majority of people who get it will have a minor case they often don’t even notice. Rather, it’s only possible to assess it in patients who are already ill—the small subset who are the most likely to die from it (especially if you evaluate the IFR in hospitalized patients).
Because of this, people came to believe the danger of COVID-19 was much worse than it actually was and until people wised up to it, a positive PCR test (which in many cases had no correlation to one becoming ill) was a source of great anxiety for the individual with that positive test.
Fortunately, because of the data which was available from widespread antibody testing (which can often determine if someone previously had COVID-19—regardless of if they developed symptoms) one of the world’s leading researchers was able to determine an accurate IFR for the disease. This to the best of my knowledge has never been done for influenza.
To quote the October of 2020 publication:
I included 61 studies (74 estimates) and eight preliminary national estimates. Seroprevalence estimates ranged from 0.02% to 53.40%. [The IFR] ranged from 0.00% to 1.63%, corrected values from 0.00% to 1.54%. Across 51 locations, the median COVID-19 infection fatality rate was 0.27% (corrected 0.23%): the rate was 0.09% in locations with COVID-19 population mortality rates less than the global average (< 118 deaths/million), 0.20% in locations with 118-500 COVID-19 deaths/million people and 0.57% in locations with > 500 COVID-19 deaths/million people. In people younger than 70 years, infection fatality rates ranged from 0.00% to 0.31% with crude and corrected medians of 0.05%.
What this essentially meant was that for most people, they had a fairly low chance of dying, and that in many places COVID was already over halfway over and we could get back to our normal lives.
Since no one in the pandemic industry benefits from that, Ioannidis’s paper was attacked, and we instead enacted the disastrous vaccination campaign (which appears to have prevented the global population from developing herd immunity to COVID-19 and thus making it possible to sell yearly vaccines to everyone). Fortunately, as time has progressed, COVID-19 has followed the normal course of an infectious virus and mutated to less and less dangerous variants. Likewise, more data has become available, allowing Ioannidis (using 40 studies from 38 countries), on January of 2023 to produce an updated estimate of the IFR (for those who had never been infected or vaccinated):
The IFRs had a median of 0.034% for the 0–59 years old population, and 0.095% for the 0–69 years old. The median IFR was 0.0003% at 0–19 years, 0.002% at 20–29 years, 0.011% at 30–39 years, 0.035% at 40–49 years, 0.123% at 50–59 years, and 0.506% at 60–69 years. IFR increases approximately 4 times every 10 years. Including data from another 9 countries with imputed age distribution of COVID-19 deaths yielded median IFR of 0.025–0.032% for 0–59 years and 0.063–0.082% for 0–69 years. Meta-regression analyses also suggested global IFR of 0.03% and 0.07%, respectively in these age groups. The current analysis suggests a much lower pre-vaccination IFR in non-elderly populations than previously suggested. Large differences did exist between countries and may reflect differences in comorbidities and other factors.
Note: another large antibody study (from Denmark) calculated an IFR of 0.18%.
These are all very low figures in line with many of the influenza estimates (0.09%-0.2%). However, they can’t actually be compared because most of the influenza ones come from datasets of active cases which inevitably overestimate the IFR. As a result we have to find different ways to look at this question.
One study, published in JAMA (an orthodox medical journal) assessed 5,212 patients in Switzerland hospitalized with COVID-19 (specifically with Omicron variant) between January 2022 to March 2022 to those hospitalized for the flu between January 2018 to March 2022. It found 4.4% of the flu patients died while 7% of the COVID-19 patients died, which was a reduction from the first half of 2020 (where the COVID death rate was 12.8%).
Another study from Turkey evaluated roughly 3,100 patients seeking help from a doctor and close to 600 who had been hospitalized, 30% of whom were infected with the Alpha variant (B.1.1.7)—which was one of the early and more dangerous variants. For those under 70, the CFR was 0.84% for those without the alpha variant and 5.3% for those with it, while for those over 70, the CFR was 31.5% for those without the alpha variant and 13.6% with the alpha variant.
Finally, a 2023 study looked at the death rates for hospitalized COVID patients with each variant:
The death rate during dominant period of Alpha, Delta, and Omicron were 5.3%, 7.5%, and 9.0% respectively and the overall death rate for all periods combined was 5.8%.
Given how messy all of this data is once you look at it under a microscope, it’s impossible to make any definitive conclusions about it. However, almost everything I’ve seen is consistent with the notion that COVID originally was a few times more deadly than the flu, but the current variants (along with improved methods of treating it) have made COVID’s IFR be fairly close to that of a flu.
Likewise, this has recently been shown by the weekly deaths the CDC has attributed to COVID-19:
Note: the closest graph I’ve found to compare this to is the one I used earlier which can be found within this article. Assuming there is not a significant spike in COVID-19 deaths over the winter (which might happen), the deaths attributable to COVID-19 are now in the same range as those typically ascribed to the flu.
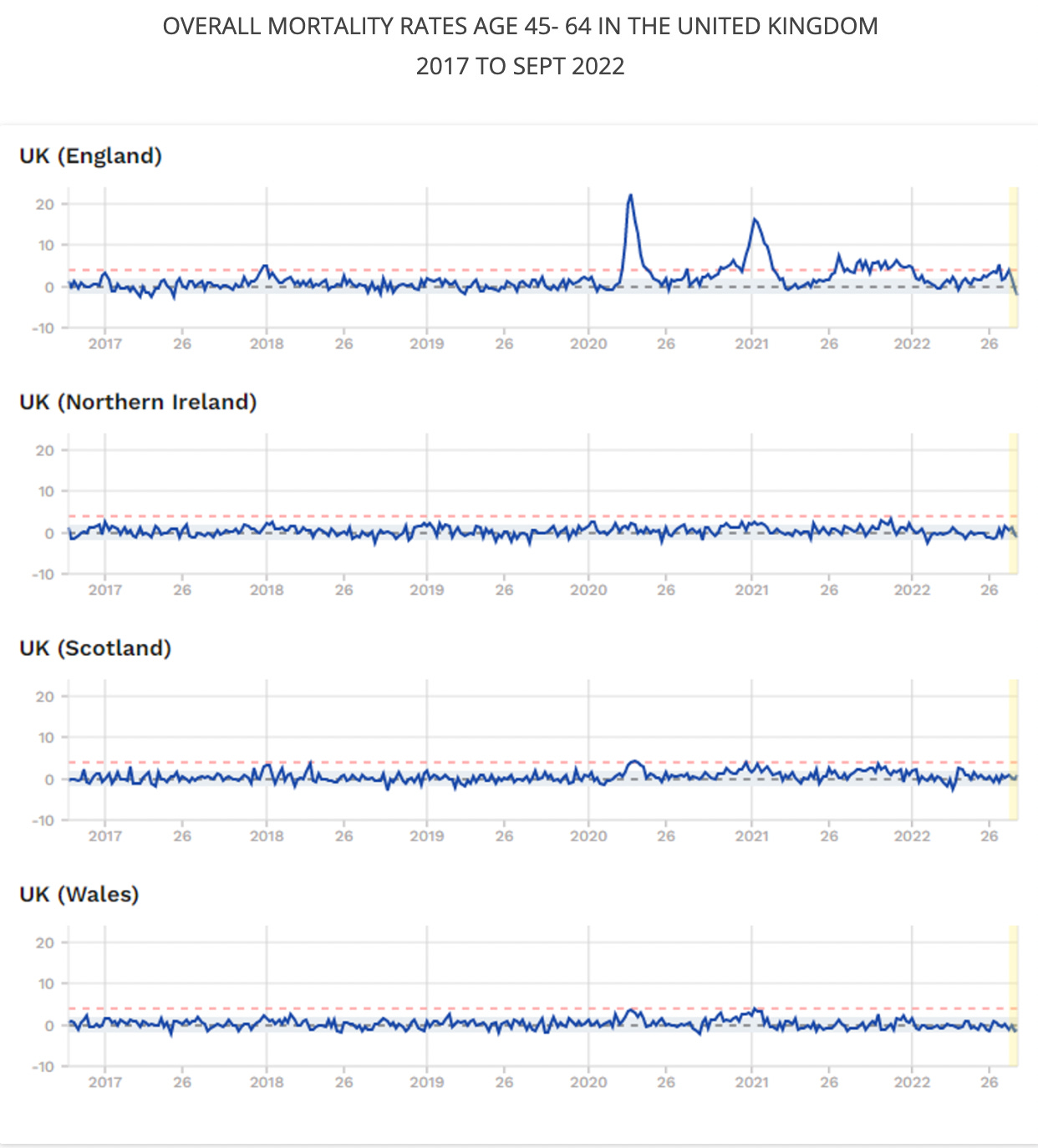
Excess Mortality
Since it is so easy for a death to be classified as one thing or another (e.g., I am relatively certain some of the deaths we classified as being due to COVID would have happened anyways and been labeled as flu deaths had COVID-19 never happened), it becomes necessary to a have a method of looking at this question which is free of that bias. The most reliable approach is to see if the total number of people who died increased, something which has occurred at a few key points during COVID, and also to lesser extents during the influenza pandemic. Consider for instance the USA’s data:
The major issues with this approach are:
•It’s impossible to know which thing actually caused the excess increase in death (e.g., a good case can be made that the lockdowns or the vaccines killed more people than COVID-19). However, when excess mortality data is presented, this is never acknowledged and the increase in it is always attributed to the prevailing narrative.
•You can adjust the predicted number of deaths for a time period to alter the assumed effect on mortality. So if the published model (arbitrarily) decides less people were expected to have naturally died during the specified time period, it makes any increase in deaths at the time appear much more significant. Conversely, if it does the opposite and decrees a higher number of deaths were expected to occur anyways, this can hide the effect of something killing people (e.g., a deadly vaccine being given to the population). For this reason, it’s often best to look at the overall trend for numerous the preceding years to determine if there does seem to be an increase or decrease in deaths at the period of time in question.
England’s data helps to illustrate these conundrums, as an obvious spike in mortality occurred during the time COVID-19 was thought to peak. Yet, that same spike was not seen in neighboring countries which had similar populations and followed similar pandemic protocols. This again illustrates how variable COVID-19 was (in some places it was catastrophic, in others it was just a flu) and how little we still know about what actually happened over the last four years.
Note: after I published this article, I sought out Pierre Kory’s perspective on all of this. Like me, it’s been quite rare for him to see patients who were hospitalized primarily for the flu; instead the majority of them had an existing chronic illness that were hospitalized for that may have been exacerbated by the flu. However, he also emphasized an important point people do not appreciate on the flu vs. COVID debate. Because COVID has an aerosol transmission (which means it spreads rapidly from person to person) rather than a droplet spread (which entails it spreading much more slowly and makes it much easier to reduce the transmission of) this resulted in a large number of people catching it very quickly.
For this reason, you would see hospitals periodically get flooded with COVID patients when the disease swept through the community, something he had never seen happen with the flu. Since my local hospital is in a significantly more rural area than the part of the midwest where Kory worked during the pandemic, while I did periodically see patients who were hospitalized for COVID, we never had a flood of them because there was not a large enough pool of people for a surge in infections to emerge when COVID spread through the community.
In contrast to our experiences, many of my colleagues in New York City (which already had issues with influenza surges during the winter due to the existing demographics) regularly had their hospitals become overloaded with COVID patients and repeatedly saw those waves in real time as over the course of a week, the number of people who showed up for COVID would significantly increase day by day until the current wave had passed.
Conclusion
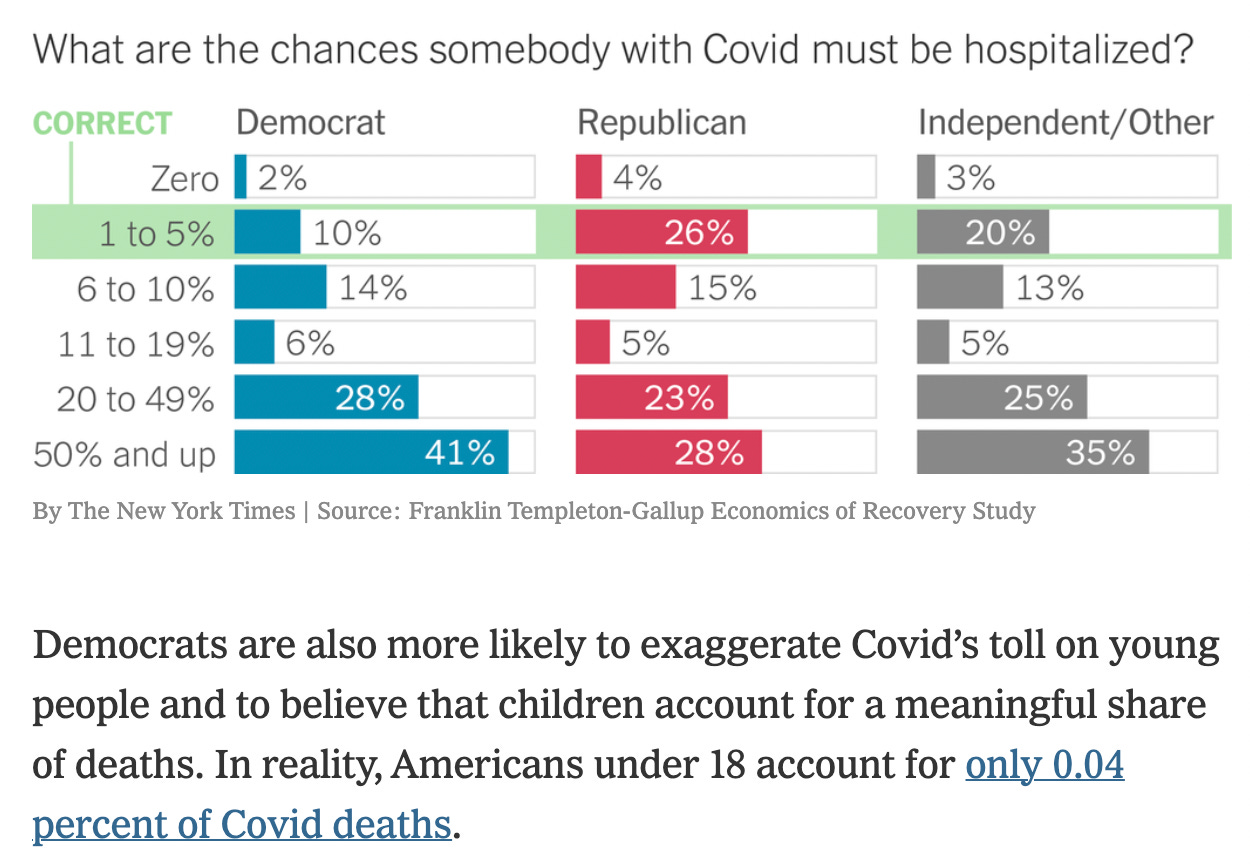
One of the great ironies with COVID-19 has been the fact that every health care authority has rallied against misinformation—yet the reality has been that the statistics underlying most of our assumptions about the pandemic are largely founded upon faulty data trying to pass itself off as objective truth.
For example, the devastating lockdowns we saw across the globe were enacted by our leaders because they had received dire warnings about what would happen if we did not lockdown—as all of the “leaders” in the public health field insisted from the start that COVID-19 had an IFR of 0.9%-1% (despite almost no evidence existing to support that contention). Yet when those (highly suspect) predictions were eventually compared to real life results, it was discovered they massively overestimated how many people would die (ranging from being off by a factor of 3 to a factor of over 10,000). Yet, there has never been any accountability for this disastrous mistake.
Likewise, a March 2021 survey, found the general public, especially those politically primed to fear the virus, also fell victim to the misinformation promoted by our healthcare authorities:
Note: for many demographics, the COVID hospitalization rate was under 1%.
As the years have gone by, I’ve gained a deeper and deeper appreciation for how many of the challenges in society arise from individuals having competing viewpoints over what’s true and what things should be done.
In turn, the success of societies is measured by their ability to have a fair way to resolve those disputes—for instance, this essentially describes how the legal system transformed society (as prior to it the one with more power typically decided both of the previous—even when those decisions were highly detrimental to the entire society).
Presently, one of the most valuable tools we have for resolving divergent beliefs is the scientific method, and allowing those disputes to be settled through scientific evidence and scientific debate. In turn, I would argue much of the success of our current society has arisen from its widespread endorsement of the scientific method. Unfortunately, this in turn has created the incentive for those seeking power to buy out the science and turn it into an opaque dogma we all follow on the basis of their “scientific” authority—the polar opposite of what science is.
In this article, I chose to try and illustrate just how little we actually know about many of the fundamental “facts” (e.g., how dangerous is the flu) that public health bureaucrats have used to usurp control over our lives, particularly throughout COVID-19, as that ambiguity was always utilized to arrive at a conclusion which benefitted their aims.
It is my sincere hope that by making the actual data available to the public alongside the context within which to interpret it, it can help to empower the public to become active participants in the scientific discourse and break the stranglehold this predatory industry has gradually gained over all of us. I thank each of you for your continued support of this newsletter and providing me with the opportunity to do something to help in this time of need.
Lastly, if you have any other subjects you wish to explore, please chime in on the October open thread (this month’s thread explored the multiple travesties with a Nobel Prize being awarded for the COVID vaccines).







Can I make a suggestion? Can you pin a thread in the comments for people to add links/citations for research they believe is relevant/enlightening? I'm tired of wading through snarky replies when I only want the references to research for myself.
I’ve been an uncritical recipient of the flu shot for the last 29 years. In the last 10 years, I’ve had two terrible bouts of the flu that resulted in ruptured eardrums, even though I had received the flu shot. Having watched the lies told about the safety and efficacy of the Covid vaccine, this year i went searching for the efficacy and safety of the annual flu shot and found your piece on Mercola’s substack a few days ago. Thank you for taking the time to research and write it and thank you for taking the time to research and write your other insightful pieces. It’s so refreshing and heartening to find thoughtful, well researched, medical information.